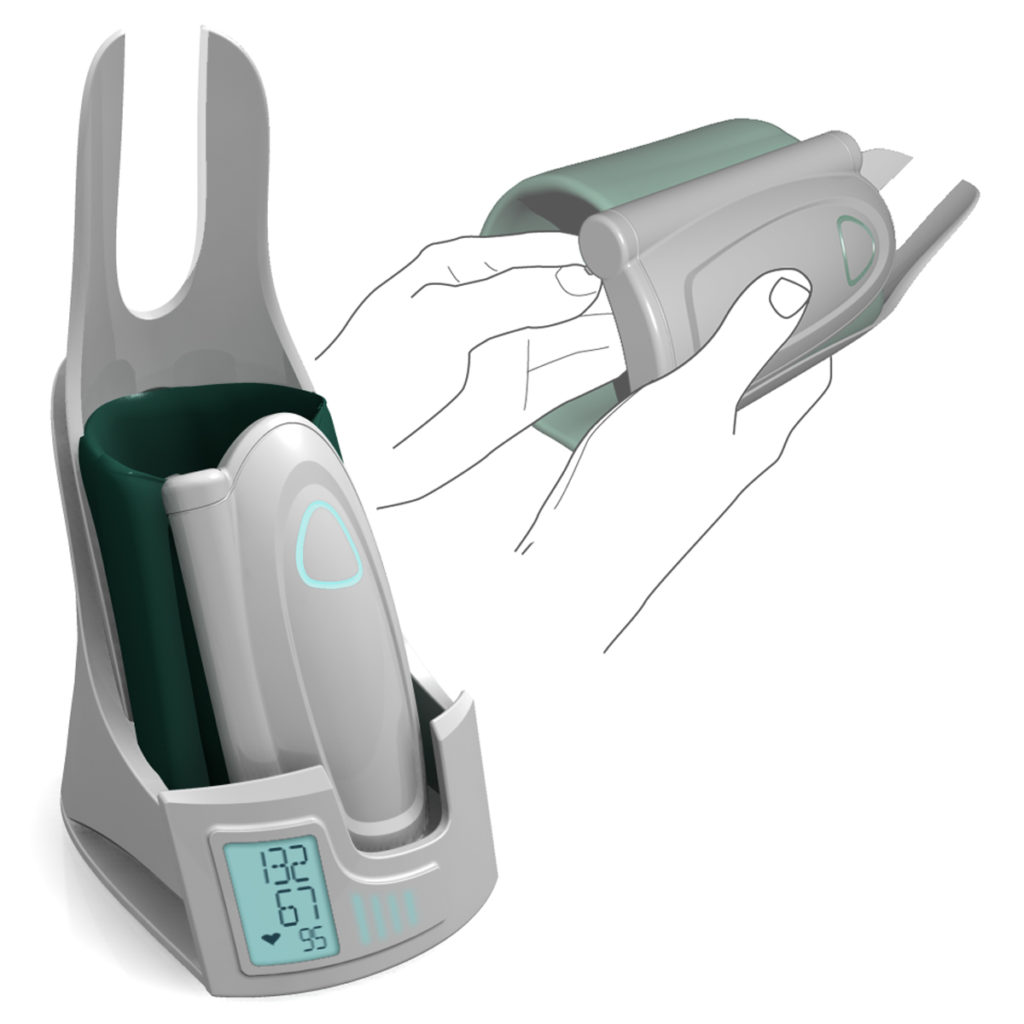
Tmeter Pressure Monitor
As I reached my final year at the Cleveland Institute of Art, I had to decide what I wanted to base my thesis on. Many other students designed cars, and while I was also very interested in cars, what I had heard about the industry had turned me off to it. Other students designed shoes or toys, none of which interested me. Instead I decided to switch my focus and set myself yet another challenge, one which would require a lot of research and which was in a field I had no previous experience in: healthcare.
I love doing research: it allows to understand a topic 360. Around me, I noticed that the focus, sometimes the starting point, was aesthetics. To me, before you try to make it look good, you need to make sure that it fulfills the needs. Beyond aesthetics, I also wanted to work on a project that could make a difference in the life and health of others. The more I researched it, the more I realized that this simple medical measuring device would regularly cause measuring discrepancies, in effect it was not reliable and life decisions were made based on these – sometimes inaccurate – results.
The year was 2005 and the internet was starting to become a good research resource, but I also looked at the history, the market, searched for complaints, purchased several pressure monitors to study them, and went to the Cleveland Clinic which is one of the largest heart centers of the world, to discuss with the specialists.
What I discovered was that there were two major causes for measurement error. One was that the placement of the sleeve was often incorrect: the sensor has to fit at the precise spot where the brachial artery splits into two. It is the increased volume at this intersection that gives a flow which is strong enough to be measured. In addition, if the arm is stretched, the flow is limited, and if it is higher than the heart, the flow pressure will also be weaker.

The second common measurement error is called “white coat hypertension”, and is simply caused by the fact that, quite often, patients who are in a medical environment become stressed, which raises their heart rate artificially, and the measure becomes again inaccurate. This is not due to the fact that it is not measured well, but rather that it is not representative of a patient’s pressure in normal conditions. Of course, a patient can measure their own blood pressure at home, but there is no certainty that it will be measured well, that the patient will be truly relaxed, in the correct position, and there is also a potential added stress when looking at the numbers and comparing them.
It seemed essential to me to solve both causes. Through my research, I discovered that no matter the gender or age of a person, the brachial artery splits at a very similar distance from the elbow. Thus, I decided to make it such that the elbow would determine where the measure would be taken. By giving it a slight angle, I removed the possibility of the arm being stretched and this would also require the patient’s position to be such that the arm would be lower than the heart.
To solve the white coat hypertension problem, I designed the measuring part of the device in such a way that it would not display the result, but rather that it would potentially appear once replaced in its charging base. The potentiality here is that the patient might or might not receive the information, depending on their preference or general tolerance to measuring stress, but rather that the result would be sent directly to their doctor. This would allow your specialist to follow your progress and you to remain at home without the stress that could impact your physiology negatively. In 2005, there were cell phones, but no iPhones and text messaging was in its infancy, thus the concept of transmitting data directly to a healthcare provider was groundbreaking.
Of course, in order to make it a medical measuring device worthy of the name, the materials I chose were medical grade plastics, which are such that they do not absorb bacteria, and that they can be easily and regularly disinfected without denaturing their surface. The sleeve adjusts to the arm size and closes similarly to the others. My research showed further that in a relaxed position, our arms are always slightly bent, and the posture that the body would get into to fit in the sphygmomanometer would be one that is quite natural, akin to rest.
